INTRODUCTION
According to the WHO, annually, 5–6% of children are born with congenital anomalies, more than 300,000 of them die within the first four weeks after birth. In Russia, congenital anomalies rank second among early neonatal death causes (18.1%) [1]. In their structure, anomalies of the gastrointestinal tract occupy second place leaving the first one to heart defects. The most frequent cause of congenital intestinal obstruction is atresia. Atresia is primarily localized in the areas of “complicated” organogenesis: esophagus, duodenum, distal ileum, and ileocecal junction [2, 3]. The rate of occurrence of intestinal atresia is 1:5,000 newborns [4]. Patients with atresia of the jejunum have an increased risk of the development of a short bowel syndrome [5].
A diversity of pathomorphological variants of intestinal defects determines difficulties in the choice of surgical tactics for a certain pathology and the technique of anastomosis formation [6]. Presently, pediatric surgeons do not have a consistent opinion on the choice of methods of surgical correction of congenital intestinal obstruction.
The study was aimed to identify the structure of congenital intestinal obstruction, to evaluate the efficiency and safety of different methods of its surgical correction.
MATERIALS AND METHODS
The authors performed a retrospective analysis of 45 medical histories of children hospitalized to the surgical department of Nizhny Novgorod Regional Clinical Hospital for Children from 2011 to 2017 with congenital intestinal obstruction. The study included 21 patients (47%) with high intestinal obstruction (13 females and 8 males) and 24 patients (53%) with low intestinal obstruction (8 females and 16 males).
The etiology of congenital intestinal obstruction is presented in Figures 1 and 2.
All patients underwent surgery. Ten patients (22%) had Kimura duodenoduodenal anastomosis formed; 3 children (6.6%) underwent duodenotomy with a membrane dissection; in 4 cases (4.4%), end-to-side (n=2) and side-to-side (n=2) anastomoses were formed; and in 2 cases (6.6%), children with Ladd’s syndrome underwent Ladd’s surgery. One child with a combination of duodenal stenosis and Ladd’s syndrome underwent dissection of Ladd’s bands and duodenoileostomy.
Seven patients (15.5%) with jejunoileal atresia had adapted anastomosis formed; 5 patients (11%) had end-to-side anastomosis formed.
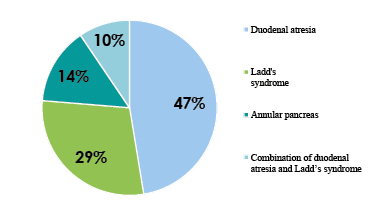
Fig. 1. Distribution of patients with high congenital intestinal obstruction by the etiology
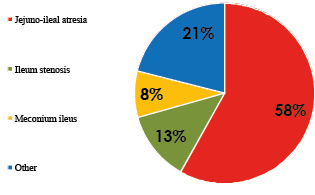
Fig. 2. Distribution of patients with low congenital intestinal obstruction by the etiology
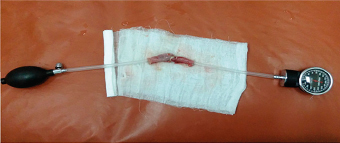
Fig. 3. Anastomosis leakage check by the method of pneumopression
Four patients (8.9%) underwent ileostomy (n=2 in patients with meconium ileus, n=2 in patients with ileal stenosis). One patient (2.2%) underwent jejunostomy. One child with a “pagoda” syndrome had de Lorimier–Harrison plication anastomosis formed. In cases with multiple intestinal atresias, end-to-end and T-shaped Bishop–Koop anastomoses were performed (2.2%).
During the experimental part of the study, the authors performed de Lorimier–Harrison ileoileal plication anastomoses to 10 male brush rabbits (n=5 – loop sutures, n=5 – continuous suture). The mean duration of the surgery was 103 + 24.9 minutes. Rabbits were narcotized with nembutal, zoletil, and novocaine. Preoperative antibiotic prophylaxis and antibiotic treatment (gentamycin) were performed for 3 days. Infusion therapy (5% solution of glucose, mexidol, 40–50 ml) was performed during the surgery. Animals were withdrawn from the experiment on Day 7 using the method of air embolism.
The study was performed according to the European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes (Strasburg, March 18, 1986, ETS No. 123). The study was approved by the local ethical committee.
The morphological study was performed using a microscope Nikon Eclipse 80 I, 10×22. Anastomosis leakage was detected by the method of pneumopression. The anastomosis area was identified. An air feeding tube was fixed to the distal end. The proximal end had a manometer attached. The pressure required for anastomosis leakage was registered (Figure 3). For the evaluation of elasticity of anastomosis, the index of stenosing (IS) was calculated by the following formula (Irvin, 1977):
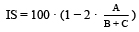 (%),
(%),
where A is the diameter of the bowel in the area of the anastomosis, B is the diameter of the bowel 2 cm higher than the anastomosis, and C is the diameter of the bowel 2 cm lower than the anastomosis.
Statistical analysis included methods of descriptive statistics with the calculations for the samplings of such parameters as arithmetical mean, median, the error of the arithmetical mean, and mean-square deviation. The significance of parametric data was evaluated using Student’s t-test and non-parametric data – Mann-Whitney U-test. The results were significant at p<0.05. The obtained values were rounded to the second decimal.
The study protocol followed guidelines for experimental investigation with human subjects in accordance with the Declaration of Helsinki and was approved by the ethics committee. Written informed consent was obtained from each patient (or official representative) before the study.
RESULTS
Among 10 operated rabbits that underwent Kimora’s duodenoduodenal anastomosing, 1 developed a complication expressed as functional anastomosis leakage. In 1 case, adhesive obstruction developed in the side-to-side anastomosis.
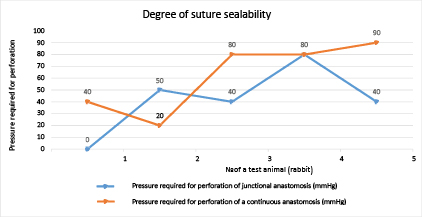
Fig. 4. A comparative evaluation of the suture sealability of junctional and continuous anastomoses
Results of the evaluation of the degree of suture sealability (junctional/continuous)
|
The pressure required for leakage (junctional anastomosis), mm Hg |
The pressure required for leakage (continuous anastomosis), mm Hg |
|
|
Mean |
42 |
56 |
|
Median |
40 |
60 |
|
Observations |
5 |
5 |
|
Hypothetical mean difference |
0 |
0 |
|
P (T<=t) one-tailed |
0.0418 |
|
After the correction of jejunoileal atresia by the method of adaptive anastomosing (n=7), 1 rabbit developed functional anastomosis leakage. End-to-side anastomosing led to 2 complications: adhesive obstruction and a combination of anastomosis leakage and adhesive obstruction.
The experimental part showed that in cases of forming de Lorimier-Harrison plication anastomosis, one-row continuous suturing had the best statistical results by the parameters of elasticity and sealability of the anastomosis (Figure 4, Table 1).
Figure 4 and Table 1 show that loop suturing was perforated in the area of anastomosis at a significantly lower pressure than continuous suturing. The mean pressure required for anastomosis leakage formed with loop suturing was 42 mm Hg, while in cases with continuous suturing, it was 56 mm Hg (p<0.05).
The evaluation of elasticity of anastomosis by the calculation of stenosing indices on Day 7 showed that in cases of continuous suturing, it was 15.2%+/–2.4%, and loop suturing – 19.1%+/–2.4%, which indicates that loop suturing is more rigid and the continuous suturing is more elastic.
The morphological study of the area of anastomosis revealed that loop suturing results in a complete lack of intestinal villi, foci of hemorrhage, necrotized masses on the surface (cellular detritus), hydropic degeneration, as well as significantly damaged epithelium and intermuscular nervous plexuses (Figures 5, 6).
In cases of continuous suturing, specific epithelium villi, goblet cells, functioning crypts, blood filling, and nervous ganglia were preserved, which indicates a lower traumatizing capacity of this suture (Figures 7, 8).
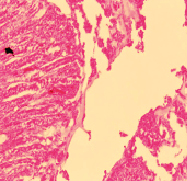
Figure 5. Histological picture of the area of anastomosis made by loop suturing (lack of intestinal villi, foci of hemorrhage)
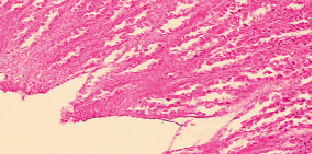
Figure 6. Histological picture of the area of anastomosis made by loop suturing (completely damaged epithelium)
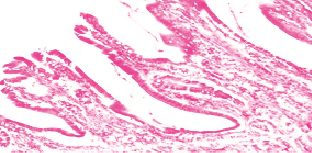
Figure 7. Histological picture of the area of anastomosis made with continuous suturing (villi with specifically preserved epithelium, goblet cells)
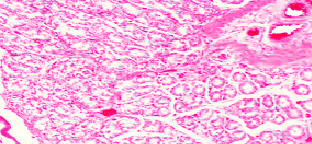
Figure 8. Histological picture of the area of anastomosis made with continuous suturing (blood filling was preserved)
CONCLUSIONS
The issue of the approaches to surgical correction for congenital intestinal obstruction remains open due to the lack of unified tactics for the treatment of this pathology. The effectiveness of the methods of surgical correction of the specified pathologies requires further study in the area of evidence-based medicine and larger samplings. The present study showed that the method of choice in the treatment for duodenal obstruction could be Kimura’s duodenoduodenal anastomosis, for a membranous type of atresia – dissection of the membrane, for jejunoileal obstruction – adaptive anastomosis, for discongruence of the intestinal segments > 4:1 – plicate anastomosis, which morphological characteristics are underdescribed in the published literature. The application of one-row continuous suture when forming plicate anastomosis increases the elasticity and scalability of the area of anastomosis and is less traumatizing. Thus, it can be recommended for the surgical treatment of children with congenital intestinal obstruction.
CONFLICTS OF INTEREST The authors declare no conflict of interest
SUPPLEMENTARY DATA (DOI)



