INTRODUCTION.
Leonard Marmor was the first to perform unicompartmental knee arthroplasty with full replacement of adjacent surfaces in femoral and tibial condyles (UKA) in 1973 [1]. Despite a good immediate outcome, orthopedic surgeons were slow to adopt this surgery [2]. The reasons for this were numerous: the ambiguity of indications and contraindications, on the one hand [3], and the far-from-perfect implant design coupled with difficult surgery, on the other hand [4]: the knee joint is anatomically and mechanically complex, which complicates this surgery.
In his overview of UKA, Bert [5] emphasizes that more and more such surgeries are done worldwide; this cumulative experience helps lower the complication rates. Long-term outcomes are leveled in elderly and working-age patients [6; 7]. A timely single-condyle replacement often stops the disease from progressing in the adjacent compartments of the joint [8; 9]. New Zealand’s and Sweden’s National Knee Arthroplasty data on endoprosthetics show that surgeons who perform 75 or more unicompartmental or total knee replacements a year face less complications in their patients [10; 11]. However, Russian surgeons still perform less UKAs than total knee replacements, mostly due to the lack of knowledge on the long-term treatment outcomes and on the factors that necessitate repeated surgery.
Research Goal. The goal hereof is to study the 15 years of UKA experience of the Russian Research Institute of Traumatology and Orthopedics n.a. R.R. Vreden, starting from the time the method was introduced up to this day; the analysis is to reveal the occurrence rates and specific nature of complications resulting in repeated surgery.
MATERIALS AND METHODS
To date, Russian Research Institute of Traumatology and Orthopedics n.a. R.R. Vreden has 17 years of UKA experience. This study covers all the patients that underwent this surgery from 2001 to 2016.
The study protocol followed guidelines for experimental investigation with human subjects in accordance with the Declaration of Helsinki and was approved by the ethics committee. Written informed consent was obtained from each patient (or official representative) before the study.
Three hundred and seventy-three UKAs were performed using a Zimmer Biomet Oxford endoprosthesis (UK), with complications arising in 28 (7.6%) of all patients. Most primary interventions were necessitated by medial gonarthrosis (306 or 82%), with osteonecrosis of the medial femoral condyle being at a far second place (67 or 18%).
Outcomes of repeated post-UKA surgeries were assessed in 100% (28) patients 7.4 years after the surgery on average (up until the end of 2016). For comprehensive analysis, the research team examined the patients, collected medical histories, clinical and X-ray data, as well as functional outcome using WOMAC and KSS scales.
RESULTS
Of the 28 patients receiving repeated surgery, most were females (23 or 82.1%) with only 5 (17.9%) males. Women were aged 62.7 and men were aged 60.8 on average. In 23 patients (82.1%), UKA was performed due to medial gonarthrosis while in 5 (17.9%) due to osteonecrosis. In most patients (26 out of 28), a unicompartmental implant had to be converted into a total one; in two patients, the endoprosthesis was preserved by arthroscopy performed to partially remove the injured lateral meniscus as well as the loose intraarticular body.
Figure 1 shows the distribution of the implants constrain.
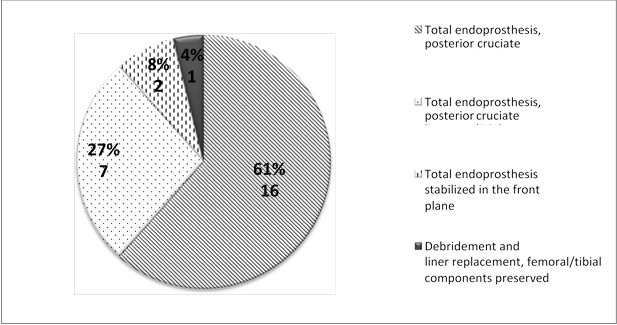
Fig. 1. Distribution of the implants used for repeated surgery by cohesion
Only 9 of 26 patients had femoral/tibial condyle bone deficiency per AORI F2A or T2a. In 3 cases, autogenous bone from adjacent condyles was enough to fill the defects; in 6 patients, 5 or 10 mm metal tibial augments were used.
Figure 2 shows the reasons why repeated post-UKA surgery was necessary.
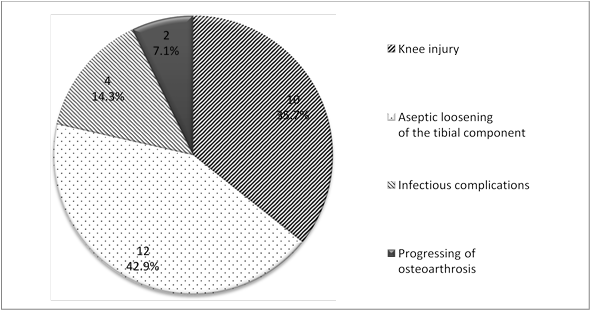
Fig. 2. Distribution of causes of repeated post-UKA surgeries
As shown in Figure 2, the aseptic loosening of the tibial component occurred in 12 or 42.9% of the patients, ranking 1st. On average, this complication developed in 4.8 years (2 to 11 years) after the first surgery.
The second most common cause was injury of various kinds, see Figure 3 for distribution.
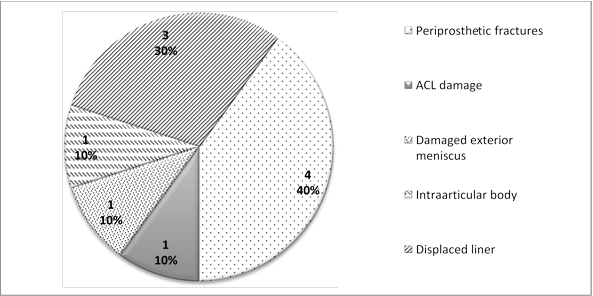
Fig. 3. Distribution of injuries that required repeated surgery
In patients with periprosthetic fractures, the inner tibial condyle was damaged more frequently than its femoral counterpart (3 cases vs 1 case, respectively), with only one component migrating as a result. The endoprosthesis was only preserved in two cases where damaged lateral meniscus was found and an intraarticular body was formed. Arthroscopy resulted in a stable positive outcome in both patients. In other cases, injuries necessitated total knee replacement. When assessing the outcome of repeated surgery using scoring systems, 26 (92.8%) patients had good scores (KSS knee score of 79, KSS function score of 87, and WOMAC = 21) while two had satisfactory scores (62, 54, and 30, respectively). No unsatisfactory outcome and no repeated re- revisions were recoded over the specified follow-up.
DISCUSSION
Analysis into the causes of repeated post-UKA surgeries over fifteen years shows that such repeated surgery is not more frequent than post-TKA surgeries. According to Swedish and Australian National arthroplasty registers, post-TKA surgery is required in 6% and 7.3% of all cases within 15 years, respectively [10]. In this study, 6.7% of unicompartmental implants had to be converted into total ones over 15 years.
Notably, while aseptic loosening of components is a common complication in any joint replacement surgery, repeated surgeries due to injuries are no less frequent: 42.9% and 35.7%, respectively, according to the data used for this research. At the same time, the New Zealand Joint Register states that the most frequent reason for post-UKA surgery is persistent pain syndrome followed by aseptic loosening of tibial and femoral components [11]. According to the Swedish Knee Arthroplasty Register, the most frequent cause is aseptic loosening while progressing osteoarthritis comes in the second place [10]. Thus, reasons for repeated endoprosthetic surgery may be region-specific due to differences in the indications and contraindications for this kind of arthroplasty while also depending on the types of implants and on the post-surgery patients’ motor activity.
While an artificial joint is expected to function for 10 years or more, it should be noted that most of the repeated surgeries covered herein (22 or 78.6%) were done within 1 to 5 years after the first surgery. However, this is in line with the international data on such patients, as the mean time to the first post-UKA surgery (if done) is 3.7 years [11]. In 4 or 1.1% of the patients, total replacement had to be performed within a year due to injuries in three of them and periprothetic infection in one. Later replacements were mostly done due to loosening of tibial component: 6 or 1.6% of the patients.
Excessive frontal deformity is a known cause of aseptic loosening: it ranged from 6º to 11º and averaged 9.25º in the patients with this complication. Thus, the continued mechanical overload of the internal knee compartment coupled with an excessive tilt of posterior tibial cut might have caused the aseptic loosening of the tibial component in the medium post-surgery term.
The joint line may change its level, another known cause of aseptic loosening of unicompartmental implants [12]. In none of the followed-up patients, its level changed by more than 1 mm compared to preoperative date, which might be due to the original surgical technique of mobile-bearing UKA.
The high occurrence rate of injuries in UKA patients is notable: 40% of injuries were periprosthesis fractures, 30% were liner displacements, 10% were damaged ligaments; 10% were damaged lateral meniscus; and in 10% cases, an intraarticular body emerged. Surveying and comprehensive medical history analysis revealed that most injuries were due to sports or physical strain. This indirectly indicates that patients preserved high motor activity in the midterm after surgery and did sports, including running and skiing. Interestingly, liner displacement is rare (only 3 cases) and has always been associated with the damage of anterior crucial ligament and medial collateral ligament in the knee, while some authors state that this complication was only the third most common one when using a mobile polyethylene bearing [13; 14] being behind loosening and progressive pathological process in other articular compartments.
Periprosthetic infection was only observed in 4 out of 28 cases: during Month 3 in 2 patients, 2 years later in one and 5 years later in another one. Two-stage tactics was applied successfully in three cases, with the infection being effectively arrested in one case by subtotal synovectomy and changing the polyethylene liner without removing the femoral and tibial components. This is consistent with most of the publications, as infectious complications are far less frequent after UKA than after TKA [15].
The rarest complication in the sample was progressing gonarthrosis in the lateral knee compartment accompanied with increasing pain syndrome (only found in 2 patients). It should be noted that converting the unicompartmental prosthesis into a total one was only necessary three years after the first surgery. This shows how important it is to carefully evaluate the condition of adjacent knee compartments when analyzing the indications for unicompartmental arthroplasty. Noninvasive scanning diagnosis (stress X-ray or MRI) must be complemented with direct imaging of the cartilage in the lateral compartment when performing preliminary diagnostic arthroscopy or carefully examining the lateral joint compartment after anteromedial arthrotomy: when there is a full-layer cartilage damage in the lateral condyles, total knee replacement is preferable, and the surgeon must be ready to perform it.
CONCLUSIONS
The causes and timing of UKA failures in the analyzed 15-year follow-up are drastically different from the data published in the international arthroplasty registers, as well as from the specific cohort follow-ups; they are also different from the complications specific to total knee replacement. Periprosthetic infection and progressing changes in adjacent joint compartments are rare while acute injuries and their consequences are only slightly behind the most common arthroplasty-related complication, i.e. aseptic implant loosening. In most cases, conversion into a total endoprosthesis can effectively use standard primary knee arthroplasty implants.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
The authors declare no conflict of interest
SUPPLEMENTARY DATA (DOI).



