Aims
The aim of the study was to investigate the parameters of sagittal vertebropelvic relations and to determine the type of vertical posture in children with bilateral high-standing greater trochanter.
Materials and Methods
The study included 30 patients (60 hip joints) aged 13 to 16 years (14.5 ± 0.9) with bilateral high-standing greater trochanter. All patients underwent routine orthopaedic examination with Harris Hip Score and Oswestry [sic: Oswestry Disability Index]. All patients underwent X-ray measurements of the parameters characterising the state of the hip joint and sagittal vertebropelvic relations.
Results
Clinical and radiological changes in the sagittal vertebropelvic relations manifest as hyperlordosis of the lumbar spine, which results from excessive pelvic anteversion. A strong positive correlation was found between the height of the greater trochanter and the slope of the sacrum – the Pearson coefficient was 0.69. Children with high-standing greater trochanter have a marked increase in global lumbar lordosis (GLL), sacral slope (SS), decrease in pelvic tilt (PT), and displacement of the sagittal vertical axis (SVA) posterior to the sacral promontory. This type of X-ray picture corresponds to the IV (hyperlordotic) type of vertical posture according to P. Roussouly.
Conclusions
The childhood anatomic changes in the hip joints are a substrate for the development of extra-articular type of femoracetabular impingement and early coxarthrosis, and compensatory changes in the lumbosacral spine predetermine the formation of mechanisms for early development of degenerative dystrophic processes.
1. Mazzini J.P., Martín J.R., Ciruelos R.M. Coxa vara with proximal femoral growth arrest as a possible consequence of extracorporeal membrane oxygenation: a case report. Cases Journal. 2009, vol. 2, no. 1, pp. 8130, doi: 10.4076/1757-1626-2-8130.
2. Pozdnikin I.Y., Baskov V.E., Barsukov D.B. Relative overgrowth of the greater trochanter and trochanteric-pelvic impingement syndrome in children: causes and X-ray anatomical characteristics. Pediatric Traumatology, Orthopaedics and Reconstructive Surgery. 2019, vol. 7, no. 3, pp. 15-24. doi 10.17816/PTORS7315-24.
3. Ganz R., Gill T.J., Gautier E., Ganz K., Krugel N., Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J. Bone Joint Surg. Br. 2001. V. 83. Р. 1119-1124.
4. Leunig M., Ganz R. The evolution and concepts of joint preserving surgery of the hip. The Bone & Joint Journal, 2014, vol. 96-B, no. 1, pp. 5-18, doi 10.1302/0301-620x.96b1.32823.
5. De Sa D., Alradwan H., Cargnelli S. et al. Extra-articular hip impingement: a systematic review examining operative treatment of psoas, subspine, ischiofemoral, and greater trochanteric/pelvic impingement. Arthroscopy. The Journal of Arthroscopic & Related Surgery. 2014, vol. 30, no. 8, pp. 1026–1041, doi 10.1016/j.arthro.2014.02.042.
6. Bech N.H., Haverkamp D. Impingement around the hip: beyond cam and pincer. EFORT Open Reviews. 2018, vol. 3, no. 2, pp. 30-38, doi 10.1302/2058-5241.3.160068.
7. Bortulev P.I., Vissarionov S.V., Baskov V.E. et al. Clinical and roentgenological criteria of spine-pelvis ratios in children with dysplastic femur subluxation. Traumatology and Orthopedics of Russia. 2018, vol. 24, no. 3, pp. 74-82, doi 10.21823/2311-2905-2018-24-3-74-82.
8. Khominets V.V., Kudyashev A.L., Shapovalov V.M. et al. Modern approaches to diagnostics of combined degenerative hip and spine pathology. Traumatology and Orthopedics of Russia. 2014, no. 4, pp. 16-26, doi 10.21823/2311-2905-2014-0-4-16-26.
9. Albers C.E., Steppacher S.D., Schwab J.M. et al. Relative Femoral Neck Lengthening Improves Pain and Hip Function in Proximal Femoral Deformities With a High-riding Trochanter. Clinical Orthopaedics and Related Research. 2015, vol. 473, no. 4, pp. 1378–1387, doi 10.1007/s11999-014-4032-9.
10. Tschauner C., Graf R. Triple intertrochanteric osteotomy in coxa vara associated with high riding of the great trochanter and leg shortening. Orthopaedics and traumatology. 1994, vol. 3, no. 1-2, pp. 88-100, doi 10.1007/bf02620396.
11. Kamosko M.M., Baindurashvili A.G. Dysplastic coxarthrosis in children and adolescents (clinic, pathogenesis, surgical treatment) [Displasticheskii koksartroz u detei i podrostkov (klinika, patogenez, khirurgicheskoe lechenie)]. St. Petersburg, SpetsLit, 2010, 72 p.
12. Hesarikia H., Rahimnia A. Differences between male and female sagittal spinopelvic parameters and alignment in asymptomatic pediatric and young adults. Minerva Ortopedica e traumatologica. 2018, vol. 69, no. 2, pp. 44-48.
13. Omeroglu H., Ucar D.H., Tumer Y.A new measurement method for the radiographic assessment of the proximal femur: the center-trochanter distance. Acta Orthopaedica et Traumatologica Turcica. 2004, vol. 38, no. 4, pp. 261-264.
14. Leunig M, Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull NYU HospJtDis. 2011, vol. 69, suppl. 1, pp. 62-67.
15. Ozer A.F. Kaner T., Bozdogan C. Sagittal Balance in the Spine. Turkish Neurosurgery. 2014. vol. 24, no. 1, pp. 13-19.
16. Zheng X., Chaudhari R., Wu C. et al. Repeatability test of C7 plumb line and gravity line on asymptomatic volunteers using an optical measurement technique. Spine. 2010, vol. 35, no. 18, p. E889-E894, doi 10.1097/brs.0b013e3181db7432.
17. Jackson R., Phipps T., Hales C. et al. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003, vol. 28, no. 2, pp. 151-160, doi 10.1097/00007632-200301150-00011.
INTRODUCTION
Hip diseases are associated with the deformities of hip components. There are nosological forms where the hip sustains a multiplane deformity, and the greater trochanter becomes high-riding. These diseases include the sequelae of acute hematogenous osteomyelitis, Perthes disease, juvenile epiphysiolysis of the femoral head, congenital and acquired varus deformities of the femoral neck. Besides, some researchers report that a high-riding greater trochanter can be a result of the suffered post-immobilization ischemic necrosis of the femoral head after a single femoral head reduction followed by rigid immobilization of the lower limbs as part of treating hip dysplasia, or after hyperbaric oxygenation is applied to a neonate, which affects the growth plates [1; 2].
Murray (1965) was the first to suggest that coxarthrosis might be connected to the anatomical change in the proximal femur. This condition was further named femoroacetabular impingement, the pathomechanics of which was detailed by Leunig and Ganz [3; 4]. Further research of this pathology identified several types of extraarticular femoroacetabular impingement, with trochanteric-pelvic impingement being the most common type [5; 6]. A high-riding trochanter that has emerged in a child will further limit the amplitude of hip movement, resulting in lameness and a progressive weakness of the gluteal muscles. Besides, a long-lasting high-riding trochanter might in some patients lead to a hip subluxation, which in turn results in pain and early coxarthrosis.
It is well-known that any change in the kinetic system comprising the hip joints and the lumbar spine may lead to anatomical and biomechanical change in the joints and in the spinal motion segments alike. Besides, the system is capable of self-overburdening, which has been described in detail for children with various spine pathologies and dysplastic hip subluxation, as well as for adults suffering from hip-spine syndrome.
High-riding greater trochanter is mainly treated surgically. Appropriate anatomical ratios are attained by corrective osteotomy of the femur or reducing the greater trochanter and resecting the femoral head; sometimes, all these methods are combined [9; 10].
However, the scientific literature available today has no data on the state of the sagittal spine-hip ratios that would determine the type of vertical posture in children suffering bilateral high-riding greater trochanter.
The goal hereof was to study the sagittal spine-hip ratios and to determine the vertical posture type in children suffering bilateral high-riding greater trochanter.
MATERIALS AND METHODS
This research involved 30 patients (60 hip joints) aged 13 to 16 (14.5 ± 0.9), all with a bilateral high-riding greater trochanter. Eighteen patients were female (60%) and 12 were male (40%). The inclusion criteria were: the age, the Risser Grade above 3, the apex of the greater trochanter being above the center of rotation of the femoral head with a shorter neck, destabilization of the hip, no femoral head deformity, no flexion contracture in the hip joints, no congenital or acquired spinal pathology, no neurological disorders, no systemic or genetic pathology, no spinal or hip surgery in the history.
The exclusion criteria were: hip subluxation or dislocation, surgical iatrogenic etiology of deformities, varus deformity of the proximal femur (neck-shaft angle <115°), and genetically verified systemic skeletal dysplasia.
Clinical examination was carried out following the standard methodology for patients with hip pathologies (Marx, 1978). To collect the most objective data on the patients’ complaints, the research team used the Harris hip score and Oswestry questionnaires. Pain syndrome severity was measured on the international visual analog scale (VAS). Radiological examination methods included hip X-ray (antero-posterior view and Lauenstein projection), as well as lateral panoramic X-ray of the spine (C1 to S1) also covering the femurs, taken off a standing patient. Radiological examination was used to calculate the Sharp and Wiberg angles, the extent of hip impingement, the neck-shaft angle, the proximal femur anteversion angle, the trochanter-to-trochanter distance (TTD), the center-trochanter distance (CTD), the thoracic kyphosis (TK) and global lumbar lordosis (GLL) degree, the pelvic incidence (PI), the sacral slope (SS), the pelvic tilt (PT), and the sagittal vertical axis (SVA).
X-ray data was evaluated in Surgimap v. 2.2.15.5. Statistical analysis was run in Excel 2010 and IBM SPSS Statistic v.23 (USA). As part of the analysis, the researchers calculated the means and the standard deviation for each indicator. Pearson’s test was used for correlation analysis.
The research was discussed and approved by the Ethics Committee of H. Turner National Medical Research Center for Children’s Orthopedics and Trauma Surgery (the Turner Center). The patients and their representatives consented to participation and publication of their personal data.
RESULTS
Upon admission to the Hip Unit of the Turner Center, 23 patients (76.7%) complained of bad gait, limited hip abduction, and pain syndrome, mainly on the posteriolateral femoral surface, experienced after walking continuously for 2 hours or after minor physical activity; they also complained about pain in the lumbar spine. Other patients (7, 23.3%) complained mainly about lameness and hip joint dysfunction. Pain syndrome in the lumbar spine would only be produced by exercising. The Harris hip score and Oswestry questionnaires returned 66.6±4.7 points and 21.5±3.7%, respectively. This suggested restrictions in the lifestyle characteristic of this age category due to hip dysfunction and pain in the lumbar spine. History analysis shed light onto what caused bilateral high-standing greater trochanter, see Figure 1.
Twenty-three patients (76.7%) developed the condition from acute hematogenous osteomyelitis survived as a neonate; 5 patients (16.7%) had it due to treatment of hip dysplasia of varying severity by Lorenz’s method, and 2 patients (6.6%) had a hypertrophic greater trochanter due to extracorporeal membrane oxygenation they had experienced as neonates.
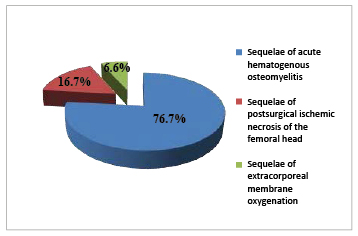
Fig. 1. High-riding greater trochanter: breakdown by etiology
Table 1
Amplitude of hip joint movements in children with bilateral high-riding greater trochanter
|
Movement |
Amplitude (M±SD) |
|
Flexion |
110±5° |
|
Extension |
5±5° |
|
Abduction |
10±5° |
|
Rotation |
15±10° |
|
Circumduction |
45±15° |
No significant (>1 cm) difference in the length of the lower limbs noted in any patient. Trendelenburg’s sign bilaterally positive in all patients.
None of the patients had frontal spinal imbalance. Adams’s test was negative in all children. Sagittal spinal profile altered in all patients as lumbar hyperlordosis. Table 1 shows changes in the goniometry of the affected hip joints.
Table 1 shows all the patients had limited abduction, extension, and rotation, as well as excessive circumduction in their hips. Impingement test was positive in 22 patients (73.3%) with an average VAS score of 3.4±1.5 in 18 patients (81.8%), 4.7±0.8 in 4 (18.2%). This corresponded to moderate pain syndrome.
Table 2 shows the results of X-ray tests (maxima, minima, and means of the Sharp and Wiberg angles, neck-shaft angle (NSA), angle of antetorsion (AA), TTD, CTD, hip impingement extent, TK and GLL degree, and sagittal spine-hip ratios).
Table 2 data suggests that the spatial position of the acetabulum, as well as the stability of the hip joints, was physiologically normal. The spatial orientation of the proximal femur was normal angle-wise; however, CTD was significantly different and TTD was slightly different from the norms [2; 13]. This indicated an anatomical deformity of the proximal femur: a shorter neck and a hypertrophic greater trochanter. TK was physiologically normal, but GLL exceeded the norm by far. Sagittal spine-hip ratios revealed differences in the positional indicators (lower PT and higher SS) as well as a pronounced SVA displacement posteriorly of the sacral promontory. Such change in the sagittal spine-hip ratios manifests itself as excessive pelvic anteversion and negative imbalance: Roussouly’s hyperlordotic vertical posture Type IV. Correlation testing revealed a strong correlation between PI and SS (r=0.89; p<0.05), GLL and SS (r=0.8; p<0.05), see Figures 2A and 2B. Besides, there was a strong positive SS-CTD correlation (r=0.69; p<0.05), see Figure 3.
Table 2
Spatial orientation values of the acetabulum, proximal femur, hip stability, sagittal spine profile, and spine-hip ratios in children with high-riding greater trochanter as compared to normal values per literature data
|
Indicators |
Patients with bilateral high-riding greater trochanter, M±SD (min-max) |
Means in healthy children (Kamosko, 2010 [11], Hesarikia et al., 2018 [12]), M±SD |
|
Sharp angle (°) |
40.1±3.4 (34–47) |
35–45 |
|
Wiberg angle (°) |
32±4.4 (26–40) |
25–40 |
|
HIE, % |
94.3±6.5 (85–100) |
85–100 |
|
NSA (°) |
135.3±5.6 (122–143) |
125–140 |
|
AA (°) |
24±6.1 (12–36) |
10–30 |
|
TTD (mm) |
59.5±9.6 (43–74.5) |
55.1±11.5 |
|
СTD (mm) |
29.4±3.6 (21.6–34) |
|
|
PI (°) |
48.4±6.4 (39.3–64.6) |
45.4±10.7 |
|
PT (°) |
–1.4±2.8 (–8.1–3.1) |
10.3±6.5 |
|
SS (°) |
49.8±5.5 (40–64) |
35.4±8.1 |
|
TK (°) |
35.6±4.2 (21.3–41) |
37.1±9.9 |
|
GLL (°) |
65.1±6.8 (56.3–87.3) |
39.6±12.4 |
|
SVA (°) |
–18.4±6.2 (–27.4–0) |
0.1±2.3 |
A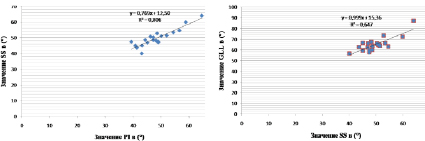 B
B
Fig. 2. Strong correlation: A: PI and SS; B: SS and GLL;
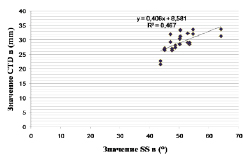
Fig. 3. Strong SS-CTD correlation
Some hip diseases are known to negatively affect the growth plates of the proximal femur, resulting in multiplane deformities. Regardless of the etiology, high-riding greater trochanter is the most common pathology, caused by damage to the growth plate of the femoral head and the upper neck edge. The person’s further growth jeopardizes the anatomy and biomechanics of the hip as the gluteal muscle attachment points grow closer, which might cause extraarticular impingement later on [14]. Clinical manifestations include gluteal muscle dysfunction, gait disorders, and pain syndrome.
To assess the state of sagittal spine-hip ratios, the researchers analyzed them in comparison to healthy children of the same age category [12].
In this research, bilateral high-riding greater trochanter patients did not differ from their healthy counterparts in terms of PI. However, PT and SS, both quantifying horizontal pelvic departure, did differ significantly. PT means were significantly lower, SS means were higher. Such values of the pelvic indices point to excessive anterior rotation of the pelvis.
In this research, the key spine-hip ratios had strong correlations, which is in line with literature data [12]. Besides, this study found a strong correlation between pelvic anteversion and the height of the high-riding greater trochanter.
Mean TK did not differ significantly in affected children vs healthy children. However, GLL was nearly twice the age-appropriate value. Analysis of SVA as a global sagittal balance characteristic showed that the patients typically had their SVA displaced posteriorly of the sacral promontory by 18.4 mm on average. Thus, the category typically had negative imbalance, because a person is considered balanced as long as their SVA is displaced by <4 mm off the gravity line [15; 16].
Roussouly’s (2003) classification of vertical postures in asymptomatic cohort helps predict the emergence and course of degenerative and dystrophic processes in the lumbar spine. Data collected herein corresponds to hyperlordotic vertical posture Type IV, which creates ground for anatomical change that will result in pathological burdening of the posterior spinal column, leading to ‘kissing’ spinous processes and in some cases to spondylolisthesis [17], see Figure 4.
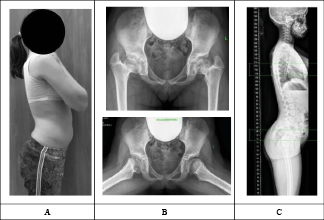
Fig. 4. Patient A, female, 13: multiplane proximal femur deformity and high-riding greater trochanter resulting from acute hematogenous osteomyelitis. A: patient’s appearance showing strong lumbar lordosis; B: X-ray image of the hip joints (PA and Lauenstein projection) showing coxaplana, a shorter femoral neck and a high-riding greater trochanter on either side; C: lateral panoramic X-ray image of the spine (C1-S1) covering the femurs, showing excess pelvic rotation anteriorly and lumbar hyperlordosis
CONCLUSIONS
Children suffering from high-riding greater trochanter have a pronouncedly stronger GLL, increased SS, reduced PT, and SVA displaced posteriorly of the sacral promontory. These changes in total manifest themselves as the excessive anterior rotation of the pelvis and lumbar hyperlordosis. Such X-ray findings point to Roussouly’s vertical posture Type IV (hyperlordotic posture). These X-ray-identified anatomical changes occurring during the childhood serve as a substrate for further extraarticular femoroacetabular impingement and early coxarthrosis, whilst compensatory changes in the spinal motion segments of the lumbar spine are fundamental to early degeneration and dystrophy. The results of this study call for further research to measure the post-operative change in sagittal spine-hip ratios and to find how corrective surgeries could be optimized.
CONFLICTS OF INTEREST The authors declare no conflict of interest
The research was carried out under Government Contract of the Russian Health Ministry No. AAAA-A18-118122690158-2.
Библиографическая ссылка
Bortulev P.I., Vissarionov S.V., Baskov V.E., Pozdnikin I.Yu., Barsukov D.B. ASSESSMENT OF THE STATE OF VERTEBROPELVIC RELATIONS IN CHILDREN WITH BILATERAL HIGH-STANDING GREATER TROCHANTER // Современные проблемы науки и образования. Хирургия. 2020. № 3. С. 22-28;URL: https://clinical-medicine.ru/ru/article/view?id=54 (дата обращения: 04.04.2025).



