Aims
The objective of the study: to demonstrate the efficacy of intraluminal endoscopic photodynamic therapy (PDT) and argon-plasma coagulation (APC-recanalisation) methods in the restoration of oesophageal patency in strictures caused by tumours in patients with locally recurrent oesophageal [sic].
Materials and Methods
Thirty patients were followed-up who underwent oesophagectomy with reconstruction using gastric (28 patients, 81.8%) and small intestinal (2 patients, 19.2%) grafts and invagination anastomosis by K.N. Tsatsanidi. All patients underwent different variants of two-level lymph node dissection. All patients were diagnosed with relapse of the disease at various times after surgery, and subsequently received systemic chemotherapy with FLOT therapeutic regimen. The main arm consisted of 11 (36.6%) patients who underwent oesophageal patency restoration by means of recanalisation of the tumour with PDT destruction. The control arm consisted of 19 (63.4%) patients who underwent palliative argon-plasma coagulation of recurrent oesophageal carcinoma. The arms were consistent and comparable in terms of the malignant disease and histological variant of the carcinoma (р< 0.05).
Results
Sessions of PDT and APC oesophageal recanalisation achieved relief of dysphagia in 100% of cases. The mean number of sessions was 4.23±0.8 for PDT and 8.25±1.7 for APC over the entire treatment period. The mean “relapse-free” period of dysphagia in PDT amounted to 3.59 weeks with PTD and 1.97 weeks with APC recanalisation. Median survival was 11.1 months in patients in the main arm and 9.8 months in the control arm.
Conclusions
Intraluminal photodynamic therapy is a safe and effective method for restoration of oesophageal patency in locally recurrent oesophageal cancer, and allows the intervals between repeated interventions for recurrent dysphagia to be increased as compared to the APR approach.
- Golyshko P.V., Novikov D.V., Anan’ev S.V. et al. A search for cancer-testis genes expression in blood and biopsy of patients with colorectal cancer [Rakovo-testikuliarnye geny v krovi i opukholi bol’nykh kolorektal’nym rakom] Russian Journal of Biotherapy - Rossijskij bioterapevticeskij zurnal, 2015, vol. 14, no. 1, pp.19-24, doi 10.17650/1726-9784-2015-14-1-19-24
- Davydov M.I., Stilidi I.S., Ter-Ovanesov M.D. et al. Esophageal cancer: current approaches to diagnosis and treatment [Rak pishchevoda: sovremennye podkhody k diagnostike i lecheniiu]. Russian Medical Journal - Russkii meditsinskii zhurnal, 2006, no. 14, pp. 1006-1015.
- Martins B.C., Wodak S., Gusmon C.C. et al. Argon plasma coagulation for the endoscopic treatment of gastrointestinal tumor bleeding. A retrospective comparsion non-treated histological cohort. United European Gastroenterology Journal, 2016, vol. 4, no. 1, pp. 49-54, doi 10.1177/2050640615590303
- Drobiazgin E.A., Chikinev Iu.V., Anikeeva O.Iu. et al. Errors and complications stenting esophagus and esophageal anastomosis [Oshibki i oslozhneniia stentirovaniia pishchevoda i pishchevodnykh anastomozov]. Journal of N.N. Blokhin Russian Cancer Research Center RAMS -Vestnik FGBU «RONTs im. N.N. Blokhina», 2016, vol. 27, no. 2, pp. 98-102.
- Godzhello E.A., Khrustaleva M.V., Permiako V.B. et al. Endoscopic stenting of the esophagus and esophageal anastomoses with self-expanding prostheses when compressed from outside [Endoskopicheskoe stentirovanie pishchevoda i pishchevodnykh anastomozov samoraspravliaiushchimisia protezami pri sdavlenii iz vne]. Herald of surgical gastroenterology -Vestnik khirurgicheskoi gastroenterologii, 2011, no. 4, pp. 22-29.
- Lozhkov A.A., Vazhenin A.V., Sharabura T.M.. et al. Reatment outcomes of external beam radiotherapy combined with high-dose-rate brachytherapy in patients with esophageal cancer [Rezul’taty sochetannoi luchevoi terapii raka pishchevoda s primeneniem brakhiterapii vysokoi moshchnosti]. Siberian journal of oncology - Sibirskii onkologicheskii zhurnal, 2017, vol. 16, no. 1, pp. 22-29. doi: 10.21294/1814-4861-2017-16-1-71-75.
- Balaz A., Kokas P., Lukovich P. et al. Palliative management of maligniant oesophageal strictures with endoprosthesis implantation. Magyar Sebészet, 2011, vol 64, no. 6, pp. 267-276, doi: 10.1556/MaSeb.64.2011.6.1.
- Best L.M. Mughal M., Gurusamy K.S. Non-surgical versus surgical treatment for esophageal cancer. Cochrane Database of Systematic Reviews, 2016, vol. 3, no. 3, p. CD011498, doi: 10.1002/14651858.CD011498.pub2.
- Massey S. Esophageal cancer and palliation of dysphagia. Clinical Journal of Oncology Nursing, 2011, vol 15, no. 3, pp. 327-329, doi 10.1188/11.CJON.327-329.
- Sigounas D.E., Krystallis C., Couper G. et al. Argon plasma coagulation compared with stent placement in the palliative treatment of inoperable oesophageal cancer. United European Gastroenterology Journal, 2017, vol. 5, no. 1, pp. 21–31, doi 10.1177/2050640616650786.
- Siersema P. Stenting for esophageal strictures. Endoscopy, 2013, vol 41, no. 4, pp. 363-373. DOI: 10.1055/s-0029-1214532.
- Seven G., Irani S., Ross A.S. et al. Partially versus fully covered self-explaining metal stents for bening and malignant esophageal conditions. Surgical endoscopy, 2013, vol. 27, no. 6, pp. 2185-2192, doi 10.1007/s00464-012-2738-x.
- Qiu G., Tao Y., Du X. et al. The impact of prior radiotherapy on fatal complications after self-expandable metallic stents for malignant dysphagia due to esophageal carcinoma. Diseases of the Esophagus, 2013, vol 26, no. 2, pp.175-181, doi 10.1111/j.1442-2050.2012.01348.x.
- Mao A. Interventional Therapy of Esophageal Cancer. Gastrointest Tumors, 2016, vol. 3, no. 2, pp. 59-68, doi 10.1159/000447512.
INTRODUCTION
Despite modern progress in oncology, among patients who received surgical and complex treatment for esophageal cancer, in 4–29% of patients, loco-regional recurrence develops, in 21–49% of patients, progressing in the form of regional lymphogenic and remote metastases [1; 2]. The main clinical manifestation of the tumor damage of the upper gastrointestinal tract is dysphagia; thus, the restoration of enteral feeding is the priority in this category of patients [3–5]. However, the majority of palliative endoscopic methods restore esophageal patency for a period of several days to a month. A week after the surgery, endoscopic recanalization without endoprosthesis (angon-plasma recanalization, bougienage) leads to the recurrence of dysphagia in 70% of patients, which is associated with hemorrhage because of malpractice in 1.5–23.7% of cases [6–8]. At the same time, the effectiveness of argon plasma coagulation (APC) in the recanalization of the obstructing tumor of the esophagus remains unsatisfactory. The lethality rate was 33.3% within 30 days after the manipulation [9; 10]. Taking into account the experience of different researchers, it is recommended to use stents in patients with a life expectancy that will not exceed 4 months [10; 11]. Besides, stenting of the esophagus leads to numerous complications (hemorrhage during the stent installation – 5.7%, stent migration – 10%, tumor restenosis – 8–57% of cases) [10–12]. Thus, the issue of safe and effective endoscopic methods in the recanalization of tumor-induced stenosis provokes disputes and requires further studies of new approaches.
The study was aimed to demonstrate the effectiveness of the methods of intraluminal endoscopic photodynamic therapy (PDT) and APC recanalization in the recovery of esophageal patency in patients with tumor strictures and local recurrence of esophageal carcinoma.
MATERIALS AND METHODS
The study included 30 patients with esophageal carcinoma that underwent endoscopic intraluminal recanalization of the esophagus for local recurrence of cancer during the period from 2013 to 2018. All patients underwent esophagectomy with extended lymph node dissection (dissection of regional lymph collector of the thoracic and abdominal cavities), esophagoplasty with a gastric (28 patients; 93.3%) and intestinal graft (2 patients; 6.7%), and the formation of invaginated anastomosis by Tsatsanidi. Intraluminal manipulations were performed between the cycles of systemic chemotherapy in the therapeutic mode FLOT (oxaliplatin, sodium levofolinate, 5-fluorouracil, docetaxel) that was indicated to all patients. The main clinical symptom of the loco-regional progression of the disease was expressed dysphagia. The main group included 11 patients (36.6%) that underwent a series of the destruction of tumor tissue by the method of intraluminal photodynamic therapy. The average age of patients in the main group was 59.0 ± 1.2 years old, the mean recurrence-free period was 14.3 months (Fig. 1). The control group included 19 patients (63.4%) that underwent a series of argon-plasma recanalization (APR) of esophageal tumor-induced stenosis. In the control group, the mean age was 62.6 ± 1.7 years old, the mean recurrence-free period was 15.6 months (Fig. 1).
In the group of PDT, tumors in the middle third of the esophagus and cardioesophageal junction were observed in 5 patients (45.5%) and tumors in the lower third were revealed in 1 patient (9.0%). In the control group, the involvement of the lower third was registered in 11 patients (57.8%), middle third – 4 (21.0%), upper third – 1 (5.3%). The spread of the tumor to the middle and lower third was registered in 3 patients (15.9%) from the group who underwent APC-recanalization (Figures 2, 3).
Tumors with T3 depth of invasion were observed in 6 patients (54.5%), T4 – in 5 patients (45.5%) from the main group. In the control group, in patients, the depth of invasion was T4 (100%) in all patients. In the main group, metastatic lymphadenopathy N3 was verified in 5 patients (45.5%), N2 – in 2 (18.2%), and in 4 patients (36.3%), lymph node metastases were not revealed. In the control group, the degree of regional metastasizing was N2 in 12 patients (63.1%) and N3 – in 7 patients (36.9%) (Table 1). By the histological variant, in the main group, low-grade and moderately differentiated adenocarcinoma was verified in 5 (45.5%) and 2 (18.2%) patients, respectively, and low-grade differentiated squamous cancer – in 4 (36.3%) of patients. In 3 (15.7%) out of 19 patients from the control group, squamous cancer pG2-G3 was diagnosed, and in 16 patients (84.3%) – moderately differentiated adenocarcinoma.
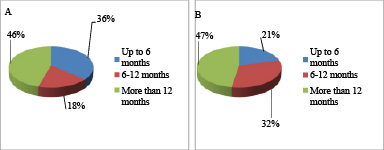
Fig. 1. Distribution of patients by the time of survival without esophageal cancer recurrence: A – in the main group (PDT); B – in the control group (APR)
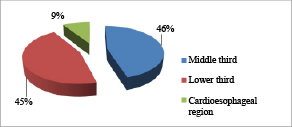
Fig. 2. Distribution of patients in the main group by the tumor localization
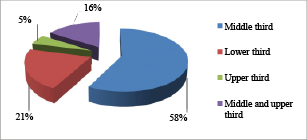
Fig. 3. Distribution of patients in the control group by the tumor localization
Table 1
Staging of the tumor process in patients with esophageal cancer in the main and control groups by the pTNM criteria according to TNM 8th ed., 2017
|
Group of patients |
T3 |
T4 |
N0 |
N2 |
N3 |
Total |
|
Main |
6 (54.5%) |
5 (45.5%) |
4 (36.3%) |
2 (18.2%) |
5 (45.5%) |
11 |
|
Control |
0 |
19 (100%) |
0 |
12 (63.1%) |
7 (36.9%) |
19 |
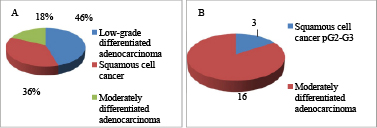
Fig. 4. Distribution of patients by the histological variant of the tumor: A – in the main group (PDT); B – in the control group (APR)
The recanalization of tumor-induced stenosis was performed by the method of intraluminal PDT. Dimeglumine chlorin E6 Fotodotazin (Veta-Grand, Ltd., Russia) was used as a photosensitizer (PS). This chlorine PS of the second generation is intended for the treatment of malignant esophageal tumors according to the nosological classification (IDC-10). A single i.v. infusion of PS at the dose of 1.0–1.4 mg/kg of body weight was given to a patient 90–120 minutes before the surgery in the conditions of a semi-dark ward and dark glasses protection. According to the pharmacokinetic properties, the maximum concentration of PS in the serum was registered in 15–30 minutes and quickly decreased. On the contrary, in the tumor, the maximum concentration of PS (10–20 µg/ml) was registered ≈ in 1 hour, and in the surrounding healthy tissues, it quickly decreased.
A semiconductor laser Latus (Atkus, Russia) was used as a source of light with the wavelength 662 ± 10 nm, area of light emission 4 cm2, laser power 8 W, time of exposure 30 minutes, cumulative effective dose 24 ± 6 J/cm2, power density 20–30 mW/cm2. A flexible light guide was delivered to the tumor by the instrument channel of Gif H180, Gif Q165 endoscopes (Olympus).
APC recanalization was performed using a high-frequency generator ERBE 300D in a Pulsed Coagulation mode, power 30–45 W, argon flow rate 2 L/min. A flexible APC probe was delivered to the area of tumor-induced stenosis via the instrument channel of the endoscope Gif Q165 (Olympus).
The study protocol followed guidelines for experimental investigation with human subjects in accordance with the Declaration of Helsinki and was approved by the ethics committee. Written informed consent was obtained from each patient (or official representative) before the study.
RESULTS
After intraluminal PDT and APR of the esophagus, all patients had temporary resolution of dysphagia. The mean number of sessions was 4.2 ± 0.8 in the PDT group and 8.3 ± 1.7 in the APR group during the period of treatment. The average disease-free time after intraluminal PDT before the recurrence of dysphagia that required repeated surgery was 25.2 days, and after APR, it was 14.1 days (p = 0.018, Log-Rank test) (Fig. 5).
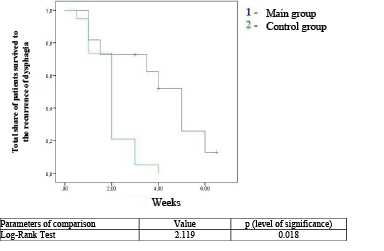
Fig. 5. Curves of time of expressed dysphagia recurrence-free survival after intraluminal interventions in patients from the main and control groups
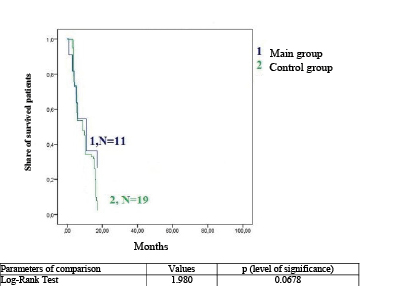
Fig. 6. Curves of Kaplan-Mayer general survival in patients with esophageal cancer in the main group (green line) and main group (blue line)
In 2 patients (10.5%) from the control group, the immediate outcome after intraluminal interventions was hemorrhage from the tumor area, which was stopped by conservative methods. Patients from the main group did not have complications and phototoxic reactions.
The differences in the general corrected survival rate in the compared groups were evaluated by the total share of the survived patients calculated by the method of Kaplan-Mayer and compared by the Log-Rank test (Fig. 6).
Besides, medians of the total survival rate depending on the applied method of local anti-tumor treatment were shown. In the group of patients that received PDT recanalization of the esophagus, it was 11.1 months. In the group of patients that underwent APC recanalization, 50% of patients survived for 9.8 months.
The comparative analysis of the general survival rate in the control and main groups did not reveal statistically significant differences (p = 0.068) (Fig. 6). Thus, there was no significant influence of the choice of the method of intraluminal treatment of tumor-induced stenosis on the survival rate of patients with recurrent esophageal cancer. Taking into account this observation, the feasibility of the choice of a palliative method of surgery of tumor-induced stenosis should be determined by the number of sessions required for the restoration of enteral feeding and quality of life of patients.
CONCLUSIONS
Intraluminal PDT is a safe and efficient method for restoring esophageal patency in patients with local recurrence of esophageal cancer that allows for an elongation of the intervals between repeated interventions for recurrent dysphagia in comparison with the APC method. Besides, it should be noted that the above-described anti-tumor methods of treatment for local recurrent esophageal cancer do not influence general life expectancy in patients.
CONFLICTS OF INTEREST
The authors declare no conflict of interest
SUPPLEMENTARY DATA (DOI)
Библиографическая ссылка
Pavelets K.V., Rusanov D.S., Protchenkov M.A., Antipova M.V., Ogloblin A.L., Karpova R.A., Pavelets M.K., Sinyavskaya O.L. CAPABILITIES OF INTRALUMINAL PHOTODYNAMIC THERAPY IN RECANALISATION OF UPPER GASTROINTESTINAL TUMOUR STENOSES // Современные проблемы науки и образования. Хирургия. – 2020. – № 2. – С. 13-18;URL: https://clinical-medicine.ru/ru/article/view?id=47 (дата обращения: 23.11.2024).



