Aims
To optimize the surgical treatment of corrosive oesophageal strictures depending on the extent of constriction.
Materials and methods
Following X-ray of the oesophagus, all patients were subdivided into groups, depending on the extent of constriction. Of the 232 patients, 143 (61.6%) had short strictures up to 4 cm, for which the method of endoscopic forced bougienage along the string-guidewire was applied. In 89 (38.4%) of patients with stricture length over 4 cm, the method of point gastrostomy was applied taking into account intraorganic anastomosis of major vascular collectors of the stomach, followed by a forced bougienage with a guide thread. The average bougienage period was 12 ± 1.3 months at intervals of 2–3 months. In addition, 19 (21.3%) of 89 patients with previously formed point gastrostomy had subtotal resection of the oesophagus with the gastric graft plasty due to bougienage inefficiency.
Results
After the first bougienage session, 138 (59.5%) patients noted regression of dysphagia from grade III to grade II. All 232 (100%) patients had restoration of food transit through oesophagus with grade I dysphagia as early as after the third session of forced bougienage. There was one death with forced bougienage with a guide thread through the previously formed gastrostomy in the patient with cachexia and aggravating multiple organ failure. The mortality rate was 0.43%. Enteral nutrition was fully restored in all patients. No signs of nutritional deficiency were noted.
Conclusions
In the event of short corrosive oesophageal stricture, the optimal treatment mode should be considered forced bougienage of the oesophagus along the string-guidewire using endoscopic guidance. With extended corrosive stenosis of the oesophagus, the method of choice is the formation of point gastrostomy with preservation of gastric intraorganic vascular line, followed by forced bougienage of the oesophagus with a guide thread. To restore the previously formed point gastrostomy, preference should be given to minimally invasive techniques. If forced bougienage is ineffective, the method of choice in the surgical treatment should be oesophagus resection with the gastric graft plasty.
- Miaukina L.M. Scar constriction of the esophagus after chemical burns. Diagnosis, tactics, treatment, prevention. Methodical recommendations [Rubtsovye suzheniia pishchevoda posle khimicheskikh ozhogov. Diagnostika, taktika, lechenie, profilaktika. Metodicheskie rekomendatsii]. St. Petersburg, 1999, 89 p.
- Godzhello E.A. Modern Concept of Treatment of Scar Oesophageal and Esophageal Anastomosis [Sovremennaia kontseptsiia lecheniia rubtsovykh striktur pishchevoda i pishchevodnykh anastomozov ]. Khirurgiia - Surgery, 2013, no. 2, pp. 97-104..
- Korolev M.P. Diagnosis and treatment of oesophageal and gastric burns [Diagnostika i lechenie ozhogovykh suzhenii pishchevoda i zheludka]. Moscow, Meditsinskoe informatsionnoe agentstvo, 2009, 345 p.
- Bulynin V.V. Tactics for the prevention and treatment of scarring oesophageal and esophageal anastomosis [Taktika profilaktiki i lecheniia rubtsovykh striktur pishchevoda i pishchevodnykh anastomozov]. Herald of surgical gastroenterology - Vestnik khirurgicheskoi gastroenterologii, 2012, no 1, pp. 16-20.
- Singhal S., Hasan S.S., Cohen, D.C. et al. Multi-disciplinary approach for management of refractoty benign occlusive esophageal strictures. Therapeutic Advances in Gastroenterology, 2013, vol. 6, no 5, pp. 365-370, doi 10.1177/1756283x13492000.
- Siersema P. Stenting for bening esophageal strictures. Endoscopy, 2009, vol. 41, no 4, 363-373, doi 10.1055/s-0029-1214532.
- Chernousov A.F. Complications of stenting in patients with benign and malignant esophageal diseases [Oslozhneniia stentirovaniia u bol'nykh s dobrokachestvennymi i zlokachestvennymi zabolevaniiami pishchevoda]. XI Congress of Surgeons of the Russian Federation: Materials of the Congress [XI s"ezd khirurgov Rossiiskoi Federatsii: materialy s"ezda]. Volgograd, Izd-vo VolgGMU, 2011, pp. 388-389.
INTRODUCTION.
Corrosive esophageal stricture caused by chemical burns is a severe complication that leads to alimentary dystrophy and disabilities. Since esophageal chemical burns are primarily observed in the young and employable population, a high social significance of the rehabilitation of such patients is evident [1]. The majority of surgeons believe that in most cases, part of corrosive strictures can be removed by different methods of gullet bougienage [1-3]. The most technically complicated and labor-consuming is the treatment of esophageal stenosis more than 4 cm long that often affects two anatomic areas. The rate of perforations of the esophagus in patients during gullet bougienage varies from 1 to 13% [3; 4]. Presently, one of the methods of treatment of post-burn strictures is the recanalization with nitinol esophageal stents [5; 6].
At the same time, esophageal stenting can be associated with severe complications: granulation stenosis, degenerative and dystrophic alterations in the mucosal layer, ingrowth of the prosthesis into the esophageal wall, and formation of ulcers and fistulas [7]. Thus, the safest and most efficient method of treatment of extended esophageal strictures remains to be gullet bougienage using a guiding thread via a preliminarily formed gastrostomy tube.
The study was aimed to optimize the surgical tactics of treatment for esophageal corrosive strictures depending on the length of the stricture.
MATERIALS AND METHODS
From 1995 to 2017, there were 232 patients with esophageal corrosive strictures caused by chemical burns that underwent treatment in the surgical department.
The study protocol followed guidelines for experimental investigation with human subjects in accordance with the Declaration of Helsinki and was approved by the ethics committee. Written informed consent was obtained from each patient (or an official representative) before the study.
The mean period from the burning to the development of the clinical symptoms of dysphagia was 60±5.6 days. The majority of patients received burns with alkaline agents. All the patients had severe dysphagia of the 3rd-4th degrees (Tables 1, 2).
Table 1
Distribution of patients by the degree of dysphagia
|
Degree of dysphagia |
3rd degree |
4th degree |
|
Total: |
96 (41.4%) |
136 (58.6%) |
Table 2
Characteristic of the damaging agent
|
Damaging agent |
Acid |
Alkali |
|
Total: |
34 (14.6%) |
198 (85.4%) |
At the first stage of treatment, all patients underwent X-ray imaging of the esophagus with a water-soluble contrasting agent for the evaluation of the level and length of stenosis and choice of the method of treatment (Figure 1). For the estimation of the length of the stricture, the authors used the classification proposed by Myaukina (1999): short (<4 cm), long (≥5 cm), subtotal and total (that affect more than two anatomical areas of the esophagus or the entire esophagus) strictures.

Fig 1. X-ray image of the esophagus with 76% solution of Urographin: extended corrosive stricture of the esophagus up to 12 cm.
In 143 (61.6%) patients with <4 cm stricture, forced bougienage was performed with a set of Salivary-Gillard bougies from No. 12 to No. 33-36 and the guiding string under the endoscopic control with i.v. sedation and 1-hour exposition. After that, control esophageal endoscopy was performed. The day after, control X-ray imaging of the esophagus was conducted. On average, for a stable clinical-X-ray effect, 3±1.25 sessions of gullet bougienage during the hospitalization were performed.
The rest 89 patients (38.4%) with extended structures had a gastrostomy tube formed by the conventional laparotomy approach considering intraorganic anastomosing of the main gastric vascular collectors, in particular, left gastric artery (LGA), right gastroomental artery (RGOA), and left gastroomental artery (LGOA) (patent No. 2417764 of May 10, 2011) for the preservation of the abovementioned vascular network and possible use of the stomach for esophagogastroplasty with further forced bougienage by the guide string (Figure 2). The guide string was fixed to a flexible guidewire 0.025 Fr in diameter and inserted in an antegrade manner by the instrumental canal of the endoscope after the guidewire, wherein it came out via the gastrostomy tube. Gullet bougienage was performed with a kit of thermoplastic bougies from No. 9 to No. 30-38 with the exposition of the last bougie not less than 1 hour. To achieve a positive clinical X-ray affect, on average, 3±1.5 sessions of gullet bougienage during the hospitalization were performed. The average time of treatment with gullet bougienage was 12±1.3 months (with sessions every 2-3 months).
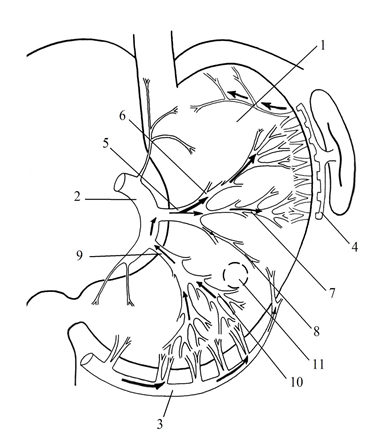
Fig 2. The localization of the gastrostomy lumen and intraorganic vascular network in the mobilized stomach: 1 – anterior gastric wall; 2 – left gastric artery (LGA); 3 - right gastroomental artery; 4 - left gastroomental artery; 5 – transverse branch of the descending section of LGA; 6 – ascending branch of the transverse branch of the descending section of LGA; 7 – mid branch of the transverse branch of the descending section of LGA; 8 – intraorganic inferior branch of the first branch of the descending section of LGA; 9 – second branch of the descending section of LGA; 10 – intraorganic superior branch of the second branch of the descending section of LGA; 11 – localization of the gastrostomy lumen on the anterior gastric wall.
The guide string was removed 12 months after the therapy after control X-ray imaging of the esophagus provided there were no signs of dysphagia and alimental dystrophy. Two months after, control esophagoscopy was conducted. In 7 patients (7.9%) with extended stricture out of 89, a repair of point-like gastrostomy tube was required using two endoscopes (patent No. 2570292 dated November 10, 2015) after a loss of the guide string with further forced gullet bougienage for 8 months with a positive outcome.
Nineteen (21.3%) out of 89 patients underwent subtotal resection of the esophagus with further gastric grafting because of the ineffectiveness of bougienage. The gastric graft was formed according to the clinically accepted method considering intraorganic anastomosing of the main gastric vascular collectors, which provided reliable blood supply to the proximal part of the gastric graft (Figure 3). The transfer of the gastric graft provides the best functional outcome in the remote period and higher quality of life for patients in comparison with patients that underwent esophagoplasty with whole gastric transposition.
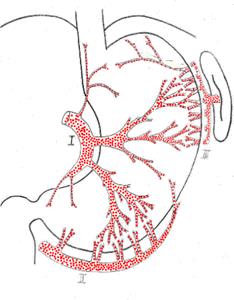
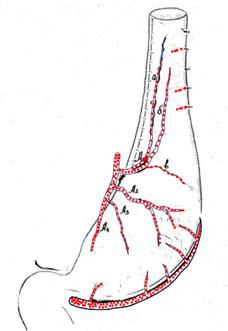
Fig 3. The layout of the formation and final view of the gastric graft.
During the formation of gastric graft, all 19 patients underwent pyloroclasia for the prevention of motor-evacuative disorders and gastric graft decompression. A nasogastric tube was inserted into the gastric graft inferior to the pyloric sphincter. After the resection of the esophagus affected by the corrosive stricture (Figure 4), the gastric graft was transferred into the right pleural cavity in the former esophagus bed, wherein the invagination esophagogastric anastomosis was formed by the method of Tsatsanidi in the upper part of the right pleural cavity. There were no registered cases of anastomotic dehiscence. After the X-ray control of the anastomosis and motor-evacuative function of GIT, the gastric tube was removed and the patient started per oral food consumption on Day 5 after the surgery (Figure 5). The average postoperative inpatient period was 10±1.78 days.
Table 3
Characteristics of the methods of treatment of patients with corrosive esophageal strictures
|
Method of treatment |
Gullet bougienage using a wireguide |
Gullet bougienage using a string guide |
Gullet bougienage using a string guide with further esophagus resection |
|
Number of patients |
143 (61.6%) |
70 (30.2%) |
19 (8.2%) |

Figure 4. Specimen of the thoracic esophagus damaged by a corrosive stricture caused by a chemical burn with acid, 9 cm long.
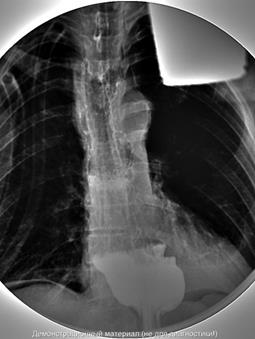

Figure 5. Control X-ray image on Day 5 after the resection of the esophagus with further gastric grafting.
RESULTS
All 232 patients (100%) recovered without complications. In 138 patients (59.5%), the first session of gullet bougienage resulted in the reduction of dysphagia from the 3rd to the 2nd degree. All 232 patients (100%) had food passage restored along the esophagus with the 1st degree of dysphagia after the third session of forced bougienage. There was one lethal outcome during forced bougienage by the guide string via a preliminarily formed gastrostomy tube in a patient with cachexia and progressing multi-organ failure. The lethality rate was 0.43%. Enteral feeding was completely restored in all the patients. There were no signs of nutritional deficit.
CONCLUSIONS.
1. In patients with short corrosive stricture, the optimum method of treatment is forced gullet bougienage by a wireguide under endoscopic control.
2. In patients with extended corrosive stricture, the method of choice is the formation of a point-like gastrostomy tube with the preservation of the gastric intraorganic vascular network and further forced bougienage of the esophagus by a guide string.
3. For the restoration of the earlier formed point-like gastrostomy tube, minimum invasive techniques should be chosen.
4. In cases when forced bougienage is ineffective, the method of choice of surgical treatment is the resection of the esophagus with gastric grafting.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
The authors declare no conflict of interest
Библиографическая ссылка
Pavelets K.V., Ogloblin A.L., Rusanov D.S., Pavelets M.K. TACTICAL ASPECTS OF TREATMENT OF CORROSIVE OESOPHAGEAL STRICTURES CAUSED BY ITS CHEMICAL BURN // Современные проблемы науки и образования. Хирургия. 2019. № 1. С. 20-24;URL: https://clinical-medicine.ru/ru/article/view?id=26 (дата обращения: 09.04.2025).
DOI: https://doi.org/10.17513/mpses.26



