Aims
The aim of this study was to analyse the immediate results of surgical treatment of patients with tumours of the lateral skull base, operated on using an en bloc resection of petrosal bone procedure.
Materials and methods
The study included 37 patients operated on for tumours of the lateral skull base in the period from 1992 to 2017. The obligatory study inclusion criterion was intracranial tumour extension. The patients were subdivided into 2 groups. Group 1 included 21 patients with malignant tumours (mainly epithelial tumours and chordomas). Group 2 included 16 patients with benign tumours of aggressive growth: paragangliomas (Fisch D1, Fisch D2, Glasscock-Jackson type IV), meningiomas grade III, giant cell reparative granuloma.) The degree of radicality in the removal of the tumour, incidence of complications and mortality and dynamics of functional state were assessed.
Results
The technique of en bloc resection of petrosal bone to the required extent allowed complete resection of the tumour in the majority of cases (71.4%) in patients with malignant tumours (group 1). The oncotomy radicality rate in group 2 was lower (37.5%), which was due to striking the balance between oncotomy extent and reduced risk of postoperative complications on account of feasibility of nonradical removal. The incidence of complications and mortality in our population of patients was 54.1% and 8%, respectively.
Conclusions
The obtained results confirm the efficacy and relative safety of en bloc resection of petrosal bone in the surgical treatment of patients with tumours of the lateral skull base.
- Gidley P.W., DeMonte F. Temporal Bone Malignancies. Neurosurgery Clinics of North America, 2013, vol. 24, no 1, pp. 97–110, doi 10.1016/j.nec.2012.08.009.
- Mazzoni A., Danesi G., Zanoletti E. Primary squamous cell carcinoma of the external auditory canal: surgical treatment and long-term outcomes. Acta Otorhinolaryngologica Italica. 2014, vol. 34, no 2, pp. 129-137.
- Heyer H. Uber einem Fall von Ohrcarcinom behandelt mit Resektion des Felsenbeines. Deutsche Zeitschrift fu¨r Chirurgie, 1899, vol. 50, no 5-6, pp. 522–533, doi 10.1007/bf02793041.
- Parsons H., Lewis J.S. Subtotal resection of the temporal bone for cancer of ear. Cancer, 1954, vol. 7, no 5, pp. 995–1001, doi 10.1002/1097-0142(195409)7:5<995::aid-cncr2820070524>3.0.co;2-a.
- Hilding D.A., Selker R. Total Resection of the Temporal Bone for Carcinoma. Archives of Otolaryngology, 1969, vol. 89, no 4, pp. 636-645, doi 10.1001/archotol.1969.00770020638016.
- Ho B., Solares C.A., Panizza B. Temporal bone resection. Operative Techniques in Otolaryngology, 2013, vol. 24, no 3, pp. 179-183, doi 10.1016/j.otot.2013.04.013.
- Homer J.J., Lesser T, Moffat D. et al. Management of lateral skull base cancer: United Kingdom National Multidisciplinary Guidelines. The Journal of Laryngology and Otology, 2016, vol. 130, no 2, pp. 119-124, doi 10.1017/s0022215116000542.
- Newlands C., Currie R., Memon A. at al. Non-melanoma skin cancer: United Kingdom National Multidisciplinary Guidelines. The Journal of Laryngology and Otology, 2016, vol. 130, Suppl. 2, p. 125-132, doi 10.1017/s0022215116000554.
- Essig G.F., Kitipornchai L., Adams F. et al. Lateral Temporal Bone Resection in Advanced Cutaneous Squamous Cell Carcinoma: Report of 35 Patients. Journal of Neurological Surgery Part B: Skull Base, 2013, vol. 74, no 1, pp. 54-59, doi 10.1055/s-0032-1331021.
- Kong J., Yang H.Y., Wang Y.F. et al. Surgical management and follow‑up of lateral skull base tumors: An 8‑year review. Molecular and clinical oncology, 2017, vol. 6, no 2, pp. 214- 220, doi 10.3892/mco.2017.1126.
- Prabhu R., Hinerman R.W., Indelicato D.J. et al. Squamous cell carcinoma of the external auditory canal: long-term clinical outcomes using surgery and external-beam radiotherapy. American journal of clinical oncology, 2009, vol. 32, no 4, pp. 401-404, doi 10.1097/COC.0b013e31818f2d48.
- Sargi Z., Gerring R., Angeli S. et al. Parotid and Temporal Bone Resection for Skull Base Malignancies: Outcome. Skull Base, 2010, vol. 20, no 3, pp. 169-177, doi 10.1055/s-0030-1247634.
INTRODUCTION.
Neoplasms in the lateral skull base represent a heterogeneous group of pathologies that differ by the source of initial growth, ways of spreading, the aggressiveness of development, and involvement of the surrounding structures in the process. From a surgical point of view, tumors of the specified localization can be divided into two groups. The first group includes tumors that are resected by step-by-step fragmenting (meningioma, paraganglioma), and the second group includes malignant tumors that require conventional surgical approaches, wherein the tumor is resected in a block with the adjoining healthy tissues. Complete resection of such neoplasms guarantees a long-term period of remission [1; 2].
Lateral skull base surgery is a relatively young and actively developing field of medicine. Even though the first successful surgeries for neoplasms in this localization were performed on the border of the 19th-20th centuries [3], for a long time, this area of neurosurgery was considered too time and effort consuming and the results were unsatisfactory. To improve the results of such surgery, some authors developed an original method called en bloc resection of the petrous pyramid that significantly influenced further development of the lateral skull base surgery [4; 5].
The aim of the present study was to analyze the short-term outcome of surgical treatment in patients with tumors of the lateral skull base that were operated by the method of en bloc resection of the petrous pyramid.
MATERIALS AND METHODS.
The study included 37 patients that had operations in different clinics for neoplasms in the lateral skull base in 1992-2017. An obligatory study entry criterion was intracranial tumor spread. The criteria of study exclusion were a low level of the functional condition of a patient (less than 60% by the Karnofsky scale) and comorbid somatic pathology at the stage of decompensation. Patients’ age varied from 18 to 73 years old (average age was 51.14±13.66).
The ratio of male and female patients was 1:1.47 (22 and 15, respectively).
Taking into account the existing differences in the biology of the tumor process, all the patients were divided into two groups. Group I included 21 patients with malignant neoplasms (primarily, epithelial tumors and chordomas). Group II included 16 patients with benign tumors with an aggressive type of growth: paragangliomas (Fisch D1, Fisch D2, Glasscock-Jackson type IV), meningiomas of Grade III, giant cell reparative granuloma.
To evaluate the outcome of the surgical treatment, the authors analyzed post-operative complications and outcomes of hospitalizations (dynamics of the clinical picture, neurological status, functional condition by the Karnofsky scale). The evaluation of the duration of the recurrence-free period was not performed.
Statistical analysis was performed using the software package STATISTICA for Windows (version 10). The study was planned based on the requirements of variation statistics. The authors used standard statistical methods of the calculation of numerical parameters of random variants including CI 95%. The evaluation of the studied parameters that characterized different accesses in the dynamics was performed with a sign test and Wilcoxon’s test. The estimation of paired statistical correlations between the parameters was performed with Spearmen’s test and Bonferroni's adjustment.
The study protocol followed guidelines for experimental investigation with human subjects in accordance with the Declaration of Helsinki and was approved by the ethics committee. Written informed consent was obtained from each patient (or official representative) before the study.
RESULTS
In Group I, the mean age of patients was 50.38±16.57 years old (from 18 to 73 years old). In Group II, the main age of patients was 52.13±11.04 years old (from 22 to 70 years old) (Figure 1).
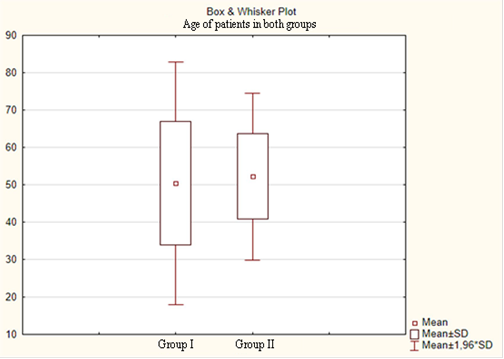
Fig. 1. Age-related parameters in both groups of patients
The analysis of groups by sex revealed the prevalence of men in Group I (57.1%) and women in Group II (81.25%) (Figure 2).
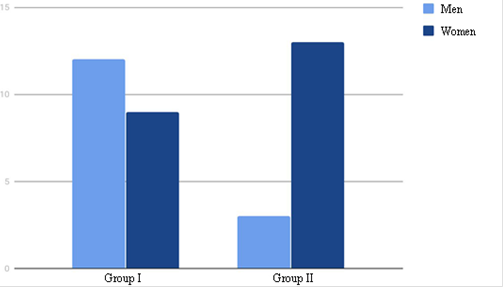
Fig. 2. The ratio of men and women in both groups.
In the group of patients with malignant tumors (Group I), squamous cell cancer (8 cases, 38.1%) prevailed. Basal cell carcinoma was registered in 5 cases (23.8%), recurrent clivus chordoma – in 5 cases (23.8%), adenocarcinoma – in 3 cases (14.3%) (Figure 3). In Group II, paraganglioma prevailed (11 cases, 68.8%). There were 4 cases (25%) of meningioma Grade III, and 1 case (6.2%) of giant cell reparative granuloma of the middle ear (Figure 4).
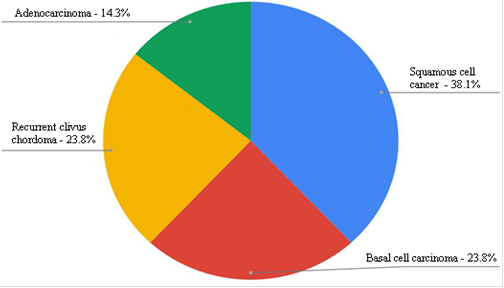
Fig. 3. Histological structure of tumors in Group I
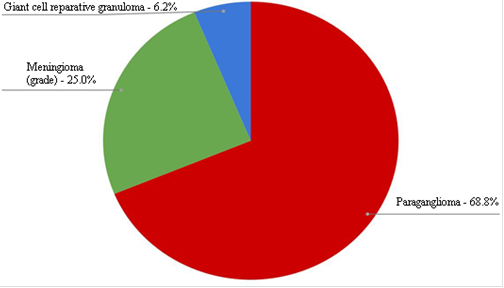
Fig. 4. Histological structure of tumors in Group II
The analysis of the frequency of surgical treatment showed that the first surgery was performed only in 3 cases (14.3%) in Group I, and in 7 cases (43.8%) in Group II. In the majority of cases, by the time of hospitalization to the clinic, patients already underwent several non-radical surgical interventions including biopsy and partial resection (Table 1).
Table 1.
Number of non-radical surgical invasions that patients underwent by the time of hospitalization to the clinic
|
Number of surgeries in the anamnesis |
Group I |
Group II |
Total |
|
1 |
11 (52.4%) |
4 (25%) |
15 (40.5%) |
|
2 |
3 (14.3%) |
4 (25%) |
7 (18.9%) |
|
3 |
3 (14.3%) |
1 (6.3%) |
4 (10.8%) |
|
4 |
1 (4.7%) |
0 |
1 (2.7%) |
|
Total |
18 (85.7%) |
9 (56.2%) |
27 (73%) |
In the group of patients with malignant neoplasms, radical types of en bloc resection of the petrous pyramid were performed (Table 2). This is explained by the necessity of complete resection of the tumor according to the principles of ablastics, which requires a safe formation of a block of tissues by the healthy borderline with its further mobilization and resection. Apart from intra-operational control, the evaluation of the radicality of en bloc resection of the petrous pyramid was performed using control post-operational CT images of the brain. The authors relied on the generally accepted criteria of the radicality of resection described in the published literature [6].
Table 2
The ratio of the volumes of pyramid resection in Group I
|
Volume of resection of the petrous pyramid |
Number of patients |
% |
|
Lateral |
2 |
9.5 |
|
Subtotal |
16 |
76.2 |
|
Total |
3 |
14.3 |
In the group of patients with benign tumors, en bloc resection of the petrous pyramid was performed primarily as an element of surgical access, which is confirmed by a lower number of radical en bloc resections in comparison with Group I (Table 3).
Table 3
The ratio of the volume of pyramid resection in Group II
|
Volume of resection of the petrous pyramid |
Number of patients |
% |
|
Lateral |
5 |
31.3 |
|
Subtotal |
10 |
62.5 |
|
Total |
1 |
6.2 |
In the present study, all the patients underwent different types of reconstruction of post-resection defects (Table 4). The necessity of this procedure is explained by the prevention of the formation of “dead space” in the area of intervention, which can be associated with an increased risk of post-operational complications that include inflammation and wound infection, liquor accumulation, and liquorrhea (in cases of dura mater defects).
Table 4
Types of reconstruction of post-resection defects
|
Type of reconstruction |
Group I |
Group II |
Total |
|
Temporal muscle |
2 (9.5%) |
2 (12.5%) |
4 (10.8%) |
|
Aponeurosis, temporal muscle, periosteum |
4 (19%) |
10 (62.5%) |
14 (37.8%) |
|
TDF on the vascular pedicle |
12 (57.2%) |
4 (25%) |
16 (51.6%) |
|
TDF with microanastomosis |
3 (14.3%) |
0 |
3 (8.1%) |
|
Total |
21 |
16 |
37 |
Note: TDF – thoracodorsal flap
En bloc resection of the petrous pyramid in the required volume allowed the surgeons to perform radical tumor resection in the majority of patients with malignant neoplasms (Table 5).
Table 5
Radicality of tumor resection in Group I
|
Degree of resection radicality |
Number of patients |
% |
|
Total (100-95%) |
15 |
71.4 |
|
Subtotal (95-75%) |
5 |
23.8 |
|
Partial (75-50%) |
0 |
0 |
|
Extended biopsy (less than 50%) |
1 |
4.8 |
Total tumor resection was considered successful when it was resected in one block within the borders of healthy tissues. This method is called clean margin resection. Such result was registered in 15 patients (71.4%) from Group I. When it was not possible technically to resect the tumor completely because of the involvement of vital vessels and neural structures in the process, the volume of resection was limited to subtotal resection (5 patients, 23.8%). In 1 case, the tumor location and previous operations did not allow the surgeons to perform the resection in the required volume.
The rate of radicality of tumor resection in Group II was lower (Table 6). This is explained by the balance between the volume of tumor resection and the decrease in risk of the post-operative deficit because, according to the published data, it is possible to perform non-radical tumor resection without a significant influence on the outcome.
Table 6
Radicality of resection of tumors in Group II
|
Degree of resection radicality |
Number of patients |
% |
|
Total (100-95%) |
6 |
37.5 |
|
Subtotal (95-75%) |
7 |
43.8 |
|
Partial (75-50%) |
3 |
18.7 |
|
Extended biopsy (less than 50%) |
0 |
0 |
To evaluate the dynamics of the patients’ condition by the Karnofsky scale, the authors chose two endpoints: hospital admission and discharge. The dynamics of this data is presented in Figures 5 and 6.
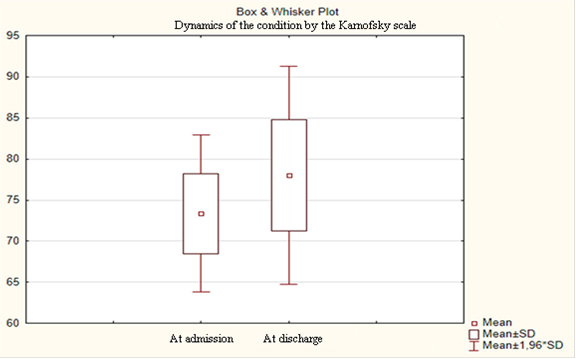
Fig. 5. Dynamics of the condition of patients by the Karnofsky scale in Group I (p<0.05)
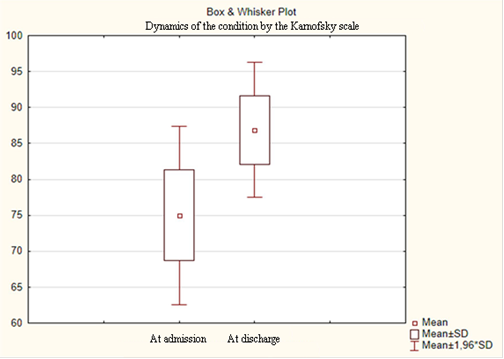
Fig. 6. Dynamics of the condition of patients by the Karnofsky scale in Group II (p<0.05)
The total amount of complications in groups is presented in Table 7. It is important to note that in Group I, some local and general complications were observed in the same patient (4 patients, 19%).
Table 7
The total rate of complications in Groups
|
Local |
General |
Total |
|
|
Group I |
11 (52.4%) |
6 (28.6%) |
17 (80.9%) |
|
Group II |
3 (18.8%) |
0 |
3 (18.8%) |
|
Total |
14 (37.8%) |
6 (16.2%) |
20 (54.1%) |
A high rate of post-operative complications in Group I is explained by several factors: the initially relatively severe condition of a patient after previous operations in the anamnesis with further radiotherapy (18 cases, 85.7%), a vast volume of post-resection cavities, and application of complicated reconstructive techniques.
The analysis of complications by groups revealed the correlation between the increase in the rate of local complications (52.4%) and the increase in the rate of using TDF for closing the post-operative defect (71.4%) in patients with malignant tumors (Table 8). On the other hand, the reconstruction of local tissues (75%) in Group II correlated with the decrease in the rate of local complications (18.8%).
Table 8
Structure of complications
|
Complication |
Group I |
Group II |
Total |
|
Meningitis |
4 (19%) |
0 |
4 (10.8%) |
|
Bleeding/hematoma |
1 (4.8%) |
0 |
1 (2.7%) |
|
Liquorrhea |
2 (9.5%) |
2 (12.5%) |
3 (8.1%) |
|
Wound infection/marginal necrosis |
7 (33.3%) |
0 |
7 (18.9%) |
|
Flap necrosis |
1 (4.8%) |
1 (6.3%) |
2 (5.4%) |
|
Neurologic impairment |
6 (28.6%) |
0 |
6 (16.2%) |
It should be mentioned that in the present study, the authors did not consider the development of the paresis of mimic structure on the side of operation after subtotal and total en bloc resection of the petrous pyramid as a complication because such manipulations are inevitably associated with the transection of the facial nerve.
The lethal outcome was registered in 3 cases (8%) in Group I.
DISCUSSION
Presently, total radical resection with or without further adjuvant therapy is considered to be a generally-accepted method of treatment for patients with tumors of lateral skull base [7; 8]. An interdisciplinary approach to this surgical problem allows the specialists to achieve satisfactory results with a relatively low level of morbidity or lethality.
Adequate reconstruction of the post-operative defect is an obligatory component of a successful outcome of the treatment with en bloc resection [6; 9]. Apart from sealing the post-resection cavity, in order to prevent the formation of “dead space”, the chosen method of reconstruction should provide maximum aesthetic qualities, which potentially influences the social adaptation of patients after the surgery.
In the present study, the rate of complications and lethality was 54.1% and 8%, respectively. The values of these parameters agree with the published data [1; 10-12].
The authors used a differential approach to en bloc resection of the petrous pyramid depending on the aim of the surgery. For patients with a malignant tumor, this method was used for the formation of a block of tissues that included the complete tumor node. Its clean margin resection agreed with the accepted practice in oncology. In the majority of patients with benign tumors, en bloc resection of the petrous pyramid was used as surgical access for adequate visualization and further mobilization of the tumor with the control of neural and vascular structures.
The present study had some limitations. First, the obtained results cannot be used as grounds for the modification of the existing recommendations because of small sampling, which is associated with a rare occurrence of this pathology and strict requirements on the intracranial spread of tumor as the study entry criterion. Second, a relatively high rate of morbidity is explained by a severe condition of patients by the time of hospitalization.
CONCLUSIONS.
The performed analysis of the experience of en bloc resection of the petrous pyramid in the treatment of patients with tumors in the lateral skull base showed that the specified technique can be considered safe and efficient. The existing methods of en bloc resection and post-operative reconstruction require further studies and improvement.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
The authors declare no conflict of interest
Библиографическая ссылка
Gulyaev D.A., Krasnoshlyk P.V., Chirkin V.Yu., Belov I.Yu., Primak N.A., Vaskova N.L., Kaurova T.A., Ivanov D.S. THE IMMEDIATE RESULTS OF EN BLOC RESECTION OF PETROSAL BONE IN THE TREATMENT STRUCTURE FOR PATIENTS WITH TUMOURS OF THE LATERAL SKULL BASE // Современные проблемы науки и образования. Хирургия. 2019. № 4. С. 4-11;URL: https://clinical-medicine.ru/ru/article/view?id=14 (дата обращения: 04.04.2025).
DOI: https://doi.org/10.17513/mpses.14



